Why do some children develop brain tumors?
 Any time a child is diagnosed with a brain tumor or other type of cancer, the most obvious question many parents ask is “why”. What caused this child to develop a brain tumor? Unfortunately, there is no easy answer to this question. Scientists now believe that the vast majority of brain tumors in children are the result of random gene mutations but have no satisfying answer as to why a particular gene mutation occurred or why it led to the growth of a brain tumor.
Any time a child is diagnosed with a brain tumor or other type of cancer, the most obvious question many parents ask is “why”. What caused this child to develop a brain tumor? Unfortunately, there is no easy answer to this question. Scientists now believe that the vast majority of brain tumors in children are the result of random gene mutations but have no satisfying answer as to why a particular gene mutation occurred or why it led to the growth of a brain tumor.
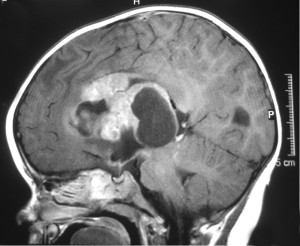
Whether benign or malignant, a tumor grows when certain cells grow, divide, and replicate more quickly than normal cells and/or they do not die when they are aged or damaged. These abnormal cells then begin to build up in the brain, forming clumps or a mass, and eventually growing large enough to press on or cause damage to the healthy brain tissue.
So why do some cells grow, function, and die normally, while others grow abnormally and develop into a brain tumor? Scientists currently believe that these abnormal cells are the result of mutations (random changes) within the DNA in each cell. Mutations in oncogenes inhibit when cells grow and divide properly, while mutations in tumor suppressor genes prevent cells from slowing their rate of replication and prevent them from dying at the proper time. Because mutations are a natural part of the lifecycle of our cells—occurring frequently as our cells grow and divide over time—preventing or predicting these mutations is currently impossible.
What are the risk factors for brain tumors in children?
A “risk factor” is anything that increases a child’s risk of developing a brain tumor. As stated above, scientists believe that the vast majority of cases of childhood brain tumors are caused by random gene mutations. Gene mutations are a natural part of human biology and usually do not have a specific or identifiable cause. Therefore, there are very few known risk factors linked to the development of brain tumors in children, with two notable exceptions. Those are:
- Radiation exposure: Exposure to large amounts of radiation has been linked to several types of cancer, including brain tumors in children. While low-level radiation exposure is an accepted aspect of today’s medical care (x-rays, for instance, for dental treatment or to diagnose a broken bone), the medical community goes to great lengths to protect children from high dosages of radiation exposure.
However, radiation therapy has proven to be an effective tool when fighting some types of cancer. While most oncologists will limit or avoid altogether the use of radiation when treating very young children, in some cases, the benefits of treating the immediate threat posed by cancer must be weighed against the potential risk of developing a brain tumor or other secondary cancer in the future.
- Inherited genetic conditions: In a very small number of cases (less than 5%), children have an inherited genetic condition that might potentially increase the risk of developing a brain tumor. Although these conditions themselves are very, very rare, some have been linked to an elevated risk for brain tumors:
- Neurofibromatosis type 1 (von Recklinghausen disease)
- Neurofibromatosis type 2
- Von Hippel-Lindau disease
- Tuberous sclerosis
- Gorlin syndrome (basal cell nevus syndrome)
- Li-Fraumeni syndrome
- Turcot syndrome
- Hereditary retinoblastoma
- Cowden syndrome
- Rubinstein-Taybi syndrome
Can we do anything to prevent a brain tumor?
Unfortunately, all too many parents—after hearing that their child has been diagnosed with a brain tumor—feel an overwhelming sense of guilt. Many wonder whether this diagnosis is somehow their fault, or whether they might have been able to do something to prevent this diagnosis. However, any oncologist will assure these parents that there is absolutely nothing they could have done to prevent their child from developing a brain tumor. Brain tumors in children are not believed to be linked to any environmental factors or lifestyle choices (with the notable exception of radiation exposure noted above); instead, they are most likely the result of random and uncontrollable gene mutations.
More about Childhood Brain Tumor Cancers:
- About Childhood Brain Tumor Cancer – Detection and Diagnosis
- Causes, Risk Factors, and Prevention of Childhood Brain Tumor Cancer
- What are the signs and symptoms of Childhood Brain Tumor Cancer?
- Childhood Brain Tumor Cancer Treatment
- Childhood Brain Tumor Cancer – Stages and Prognosis
- What is the expected life span of Childhood Brain Tumor Cancer?
- After Treatment – Living as a Childhood Brain Tumor Cancer Survivor
Learn More About the Different Types of Childhood Cancers:
- Childhood Brain Tumor Cancer (Brain Stem Tumors)
- Spinal Cord Tumor Cancer
- Childhood Neuroblastoma Cancers
- Childhood Hodgkin Lymphoma Cancers
- Non-Hodgkin Lymphoma Cancers
- Wilms tumor (Kidney Tumors)
- Rhabdomyosarcoma
- Retinoblastoma
- Bone cancer (including osteosarcoma and Ewing sarcoma)
- Leukemia Cancers: Acute lymphocytic (lymphoblastic) leukemia (ALL) Acute myelogenous leukemia (AML); Juvenile myelomonocytic leukemia (JMML)
- Hepatoblastoma (Liver Cancer)
- Rhabdoid Tumors
About American Childhood Cancer Organization
American Childhood Cancer Organization (ACCO) is a non-profit charity dedicated to helping kids with cancer and their families navigate the difficult journey from cancer diagnosis through survivorship. Internationally, ACCO is the sole U.S. member of Childhood Cancer International (CCI), the largest patient-support organization for childhood cancer in the world. Here in the United States, ACCO promotes the critical importance of ensuring continued funding into new and better treatment protocols for childhood cancer. And most importantly, ACCO is focused on the children: developing and providing educational tools for children fighting cancer and their families, empowering them in their understanding of childhood cancer and the medical decisions they must make during this difficult journey. All of ACCO’s resources are available free of charge for families coping with childhood cancer.
For additional information about childhood cancer or on the ACCO, or to order resources for you or your child, please visit our website at www.acco.org , call 855.858.2226 or visit: