Statistics on Five-Year Survival Rates for Children with Neuroblastoma
 Any discussion of prognosis or outlook is usually based on five-year survival rates, or the percentage of children with a specific type of cancer who live at least five years after their initial diagnosis. These numbers are based on studies performed at least five years ago, and so may not reflect improvement in treatment options for some types of cancers. Moreover, these numbers are merely averages and do not indicate the outlook or prognosis for your specific child. Your child’s oncologist will be able to give you a better understanding of your child’s unique case based on his or her type of cancer, age, general health, and response to treatment.
Any discussion of prognosis or outlook is usually based on five-year survival rates, or the percentage of children with a specific type of cancer who live at least five years after their initial diagnosis. These numbers are based on studies performed at least five years ago, and so may not reflect improvement in treatment options for some types of cancers. Moreover, these numbers are merely averages and do not indicate the outlook or prognosis for your specific child. Your child’s oncologist will be able to give you a better understanding of your child’s unique case based on his or her type of cancer, age, general health, and response to treatment.
Staging and Prognosis Factors for Neuroblastoma
Five-year survival rates for neuroblastoma are based on a complex system that involves a detailed understanding of the stage of the disease at diagnosis and a series of “prognosis factors”. Currently, statistics on survival rates for neuroblastoma are maintained by the Children’s Oncology Group (COG), which classifies all cases of neuroblastoma into three risk groups: low risk, intermediate risk, and high risk. These risk grouping are based the disease’s stage and prognosis factors.
Staging: There are two different methodologies to determine the stage of disease, or how far the disease has spread beyond the site of the original tumor:
- INRGSS: International Neuroblastoma Risk Group Staging System utilizes the results of imaging tests such CT, MRI, or MIBG scans and can be determined before treatment has begun.
- INSS: International Neuroblastoma Staging System assesses staging after surgery to remove the tumor is performed.
Prognosis factors: these are certain markers that can indicate whether a specific neuroblastoma may respond better or worse to treatment, and can impact a child’s long-term outlook. Specific prognosis factors used to help assign risk for neuroblastoma are:
- Age: children under 12-18 months tend to have a better long-term outlook than older children
- Tumor histology: when examined under a microscope, tumors that contain more normal-looking cells tend to have a better prognosis (favorable histology v. unfavorable histology)
- DNA ploidy: in young children, neuroblastoma cells that contain the same amount of DNA as normal cells (a DNA index of 1, or diploid) seem to respond less favorably to treatment than those that have an increased amount of DNA (a DNA index greater than 1, or hyperdiploid).
- MYCN gene amplifications: neuroblastomas with too many copies of the MYCN oncogene (a gene that helps regulate cell growth and division) seem to grow more quickly and respond less well to treatment.
- Chromosome changes: scientists are just now beginning to understand how the presence or lack thereof of certain chromosomes with the DNA structure of the cells can impact the prognosis for neuroblastoma.
- Neurotrophin (nerve growth factor) receptors: Neurotrophin is a chemical that helps nerve cells mature. Neuroblastomas that have more neurotrophin receptors, especially those receptors called TrkA, are associated with a better long-term outlook.
Five-Year Survival Rates by Risk Group (COG Risk Groupings)
Low Risk: Children whose neuroblastoma is considered “low risk” have a five-year survival rate that is higher than 95%. The low risk group incorporates children who fall into the following categories:
- All Stage 1 diagnoses
- Stage 2A or 2B and under 1 year of age
- Stage 2A or 2B, older than 1 year of age, with 0 extra copies of the MYCN gene
- Stage 2A or 2B, older than 1 year of age, with extra copies of the MYCN gene and a favorable histology
- Stage 4S with favorable histology, hyperdiploid, and no extra copies of the MYCN gene
Intermediate Risk: Children whose neuroblastoma is considered “intermediate risk” have a five-year survival rate of 90-95%. The intermediate risk group incorporates children who fall into the following categories:
- Stage 3, under 1 year of age, no extra copies of the MYCN gene
- Stage 3, greater than 1 year of age, no extra copies of the MYCN gene and a favorable histology
- Stage 4, under 1 year of age, no extra copies of the MYCN gene
- Stage 4S, no extra copies of the MYCN gene and has normal DNA ploidy and/or has an unfavorable histology
High Risk: Children whose neuroblastoma is high risk have a five-year survival rate of 40-50%.
- Stage 2A or 2B, over 1 year old, with extra copies of the MYCN gene and an unfavorable histology
- Stage 3, under a year old, with extra copies of the MYCN gene
- Stage 3, over a year old, with extra copies of the MYCN gene
- Stage 3 and over 18 months old, with an unfavorable histology
- Stage 4 with extra copies of the MYCN gene
- Stage 4 and over 18 months old
- Stage 4, between 12 and 18 months old, with extra copies of the MYCN gene, unfavorable histology, and/or a DNA index of 1
- Stage 4S with extra copies of the MYCN gene
Request for free resources here.
 More about Childhood Neuroblastoma Cancers:
More about Childhood Neuroblastoma Cancers:
- About Childhood Neuroblastoma Cancer – Detection and Diagnosis
- Causes, Risk Factors, and Prevention of Childhood Neuroblastoma Cancer
- What are the signs and symptoms of Childhood Neuroblastoma Cancer?
- Childhood Neuroblastoma Cancer Treatment
- Childhood Neuroblastoma Cancer – Stages and Prognosis
- After Treatment – Living as a Childhood Neuroblastoma Cancer Survivor
Learn More About the Different Types of Childhood Cancers:
- Childhood Brain Tumor Cancer (Brain Stem Tumors)
- Spinal Cord Tumor Cancer
- Childhood Neuroblastoma Cancers
- Childhood Hodgkin Lymphoma Cancers
- Non-Hodgkin Lymphoma Cancers
- Wilms tumor (Kidney Tumors)
- Rhabdomyosarcoma
- Retinoblastoma
- Bone cancer (including osteosarcoma and Ewing sarcoma)
- Leukemia Cancers: Acute lymphocytic (lymphoblastic) leukemia (ALL) Acute myelogenous leukemia (AML); Juvenile myelomonocytic leukemia (JMML)
- Hepatoblastoma (Liver Cancer)
- Rhabdoid Tumors
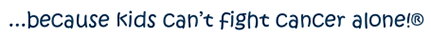


 In many cases, symptoms of neuroblastoma are caused by a tumor, or mass of cancerous cells, that becomes visible through the skin or begins to press on other organs of the body. The location of the primary tumor will impact the specific symptoms the child is experiencing. For instance:
In many cases, symptoms of neuroblastoma are caused by a tumor, or mass of cancerous cells, that becomes visible through the skin or begins to press on other organs of the body. The location of the primary tumor will impact the specific symptoms the child is experiencing. For instance:






 Neuroblastoma is caused by the abnormal development of immature nerve cells known as neuroblasts. As a fetus develops, most neuroblasts grow and eventually become mature nerve cells either before birth or in the first few months after birth. However, in some cases, neuroblasts do not develop correctly. Instead of becoming mature nerve cells, they continue to grow and divide. In some cases, these abnormal neuroblasts simply die off; however, in some rare cases, they develop into tumors or neuroblastoma.
Neuroblastoma is caused by the abnormal development of immature nerve cells known as neuroblasts. As a fetus develops, most neuroblasts grow and eventually become mature nerve cells either before birth or in the first few months after birth. However, in some cases, neuroblasts do not develop correctly. Instead of becoming mature nerve cells, they continue to grow and divide. In some cases, these abnormal neuroblasts simply die off; however, in some rare cases, they develop into tumors or neuroblastoma. Clinical trials are a part of long-term research studies designed to develop and test potential new treatment options for cancer and other illnesses. When a team of physicians and/or scientists believes they have developed a potentially effective new treatment, they will first study the treatment in the lab, and then potentially test it on animals. If the new treatment shows promise, it may be tested in people through a multi-phase clinical trial. This is an important step in determining whether a new treatment gets government approval and can be incorporated into existing treatment protocols. Clinical trials are a critical part of the on-going fight to develop new and better treatment options for cancers, especially childhood cancers.
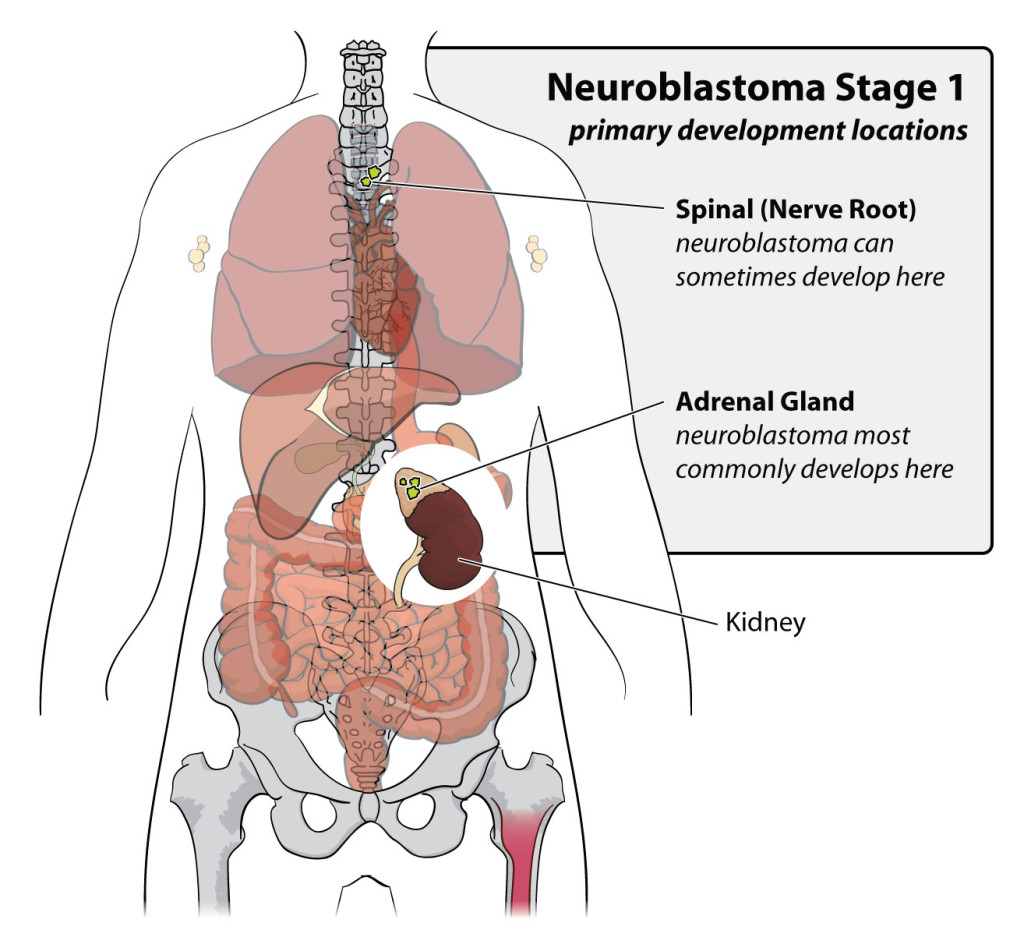
Clinical trials are a part of long-term research studies designed to develop and test potential new treatment options for cancer and other illnesses. When a team of physicians and/or scientists believes they have developed a potentially effective new treatment, they will first study the treatment in the lab, and then potentially test it on animals. If the new treatment shows promise, it may be tested in people through a multi-phase clinical trial. This is an important step in determining whether a new treatment gets government approval and can be incorporated into existing treatment protocols. Clinical trials are a critical part of the on-going fight to develop new and better treatment options for cancers, especially childhood cancers. Neuroblastoma is a type of childhood cancer that develops in immature nerve cells within the sympathetic nervous system. Part of the autonomic nervous system (which controls bodily functions we do not consciously control, such as breathing and heart rate), the sympathetic nervous system is made up of nerve fibers that run parallel to the spinal cord, ganglia (clusters of nerve cells) found along the nerve fibers, and nerve-like cells located in the adrenal glands. Neuroblastoma begins to grow in the very early forms of nerve cells as they develop in the embryo or fetus.
Neuroblastoma is a type of childhood cancer that develops in immature nerve cells within the sympathetic nervous system. Part of the autonomic nervous system (which controls bodily functions we do not consciously control, such as breathing and heart rate), the sympathetic nervous system is made up of nerve fibers that run parallel to the spinal cord, ganglia (clusters of nerve cells) found along the nerve fibers, and nerve-like cells located in the adrenal glands. Neuroblastoma begins to grow in the very early forms of nerve cells as they develop in the embryo or fetus. On average in the United States each year, there are more than 4,000 new diagnoses of
On average in the United States each year, there are more than 4,000 new diagnoses of