“Avery is a 5 year old Gold Ribbon Hero as she has faced cancer twice in her short life. She was diagnosed with Stage 2 Wilms tumor in 2012, and Stage 3 recurrent Wilms in January 2014. She has fought 5 surgeries, 10 fragments of radiation, multile transfusions, 6 months of chemo in 2012 and 7 months in 2014. She has remained incredibly strong, despite all the pain and challenges during this time. She is a true fighter and one that exemplifies strength, courage, and positivity. She has been an inspiration to many…Avery…is our hero!!” – Kari C. 
Author Archives: ACCO
Gold Ribbon Hero Avery C
Gold Ribbon Hero Kathleen P
“My hero is a special needs bus driver and a single mom to three kids. She lost her first born son to neuroblastoma. She has never given up her dream of getting her college degree and is currently is a 52 year old college student trying to obtain her degree in social work.” – Alicia P.

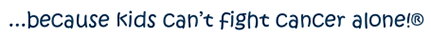
Gold Ribbon Hero Brody E
“BRODY fought hard for a year, but it wasn’t meant to be! BRODY became cancer free 4/15/14 when he gained his wings. He had brain cancer – GBM.” – Tanya E.
Pediatric Cancer Patients Treated to Free Popsicles to Fight Effects of Treatment
Nothing is better than an ice-cold popsicle on a hot summer day, especially when it’s free! If you’re a young patient coping with cancer, a freezer pop is not only a tasty treat; it also makes you feel better.
In partnership with the American Childhood Cancer Organization (ACCO) and The Jel-Sert Company, maker of Fla-Vor-Ice and Otter Pops, Nemours Children’s Clinic and The Children’s Hospital at Sacred Heart in Pensacola is now providing outpatient pediatric cancer patients with free ice pops all throughout the year as part of the “Take a Pop; Share a Smile” program. Young patients who visit Nemours Children’s Clinic and the hospital’s Pediatric Infusion Center for outpatient cancer treatment are invited to choose a pop in their favorite flavor.
 Jel Sert and the ACCO recently donated a 5-cubic-foot freezer to Nemours Children’s Clinic and stocked it with 200 freezer pops. The Jel Sert Company will keep it stocked with a continuous supply of pops.
Jel Sert and the ACCO recently donated a 5-cubic-foot freezer to Nemours Children’s Clinic and stocked it with 200 freezer pops. The Jel Sert Company will keep it stocked with a continuous supply of pops.
Children with cancer face many challenges, including several unpleasant side effects from treatment. Invasive, toxic therapies can cause painful mouth sores, which make eating, drinking and even speaking difficult. Ice pops are often used to ease the pain and to bring some fun into a very serious situation. They are a welcome source of oral hydration, too. Whether a child with cancer is visiting for lab work or undergoing treatment, he or she is invited to choose a pop.
“Little things like an icy-cold freezer pop can make a big difference to a child coping with cancer,” says Jenny Greunke, pediatric social worker with Nemours Children’s Clinic. “The freezer design is colorful, and getting these free, icy treats just adds a little fun to their treatment visits,” says Greunke.
The “Take a Pop; Share a Smile” program began in 2008, and today almost 90 children’s hospitals and pediatric treatment facilities across the U.S. are partners. For more information about this program, visit www.jelsert.com.
Click Here to See The News Story





Gold Ribbon Hero Lucas S
“My son Lucas was a fighter since we first found out on September 28, 2012 that he had ALL. He gave it his all until his final breath on Jun 28, 2014. My baby is my hero and always will be. He went into remission Oct 29, 2012 but relapsed March 11, 2014. He received a bone marrow transplant May 28, 2014 but due to complications from the high doses of chemo and radiation his little body just couldn’t fight anymore. He has touched the lives of many and in his honor I think he deserves a Gold Ribbon.” – Robin S.

Go Gold® 2014 Awareness Shirt Names
Go Gold® for Kids with Childhood Cancer Shirts
Below are the images with the list of names for the 2014 Childhood Cancer Awareness Shirts. We are unfortunately not able to make any further corrections or additions. Please be sure to email us at cperry@acco.org to add your child’s name to our next project.
Campaign Is Over (For Now)
Click Here to Order Adult Shirts
Gold Ribbon Hero Nathan A
“Nathan just completed his cancer treatment. He is now cancer free. #nathansfight” – Lizzette A.

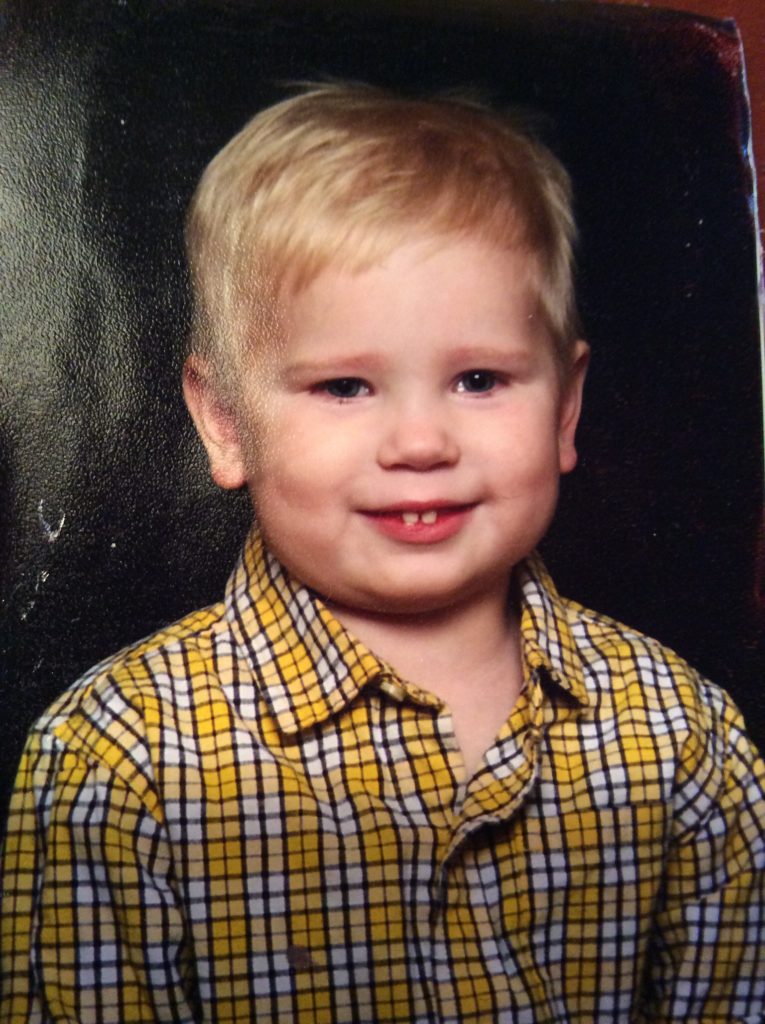
One Hundred Percent
100% – Is What the Survival Rate Should Be For All Kids with Cancer
DAY 7: KIDS ARE NOT JUST LITTLE ADULTS
If your child spikes a fever in the middle of the night, do you give him two adult ibuprofen tablets with a glass of water? No, instead you reach for the bottle of children’s ibuprofen because you know the adult tablets could be harmful to him. If your child is in pain because she has broken a bone playing soccer, do you relieve her distress with vicodin or oxycontin? No, because again, you know that they could be harmful, or even toxic, for her. And yet, when a child falls ill with childhood cancer, we don’t question giving that child the same medications and treatments we would give to an adult suffering from an adult form of cancer. Cancer treatments for adults have made remarkable, even miraculous breakthroughs in recent days, but using these cookie-cutter treatments on children instead of investing in new lines of research means that those successes have not been mirrored in survival rates for childhood cancers. As one mother pointed out, “Everywhere I look, I see pink ribbons and I feel thankfulness—and I feel anguish. According to an article published in the New York Times on September 22, 2008, as a result of advances in treatment, ‘98 percent of women with early-stage [breast] cancers survive at least five years…’ Why is this true? Because we have banded together to raise awareness and funding for our mothers, our sisters, our aunts, and our daughters. Our children who are living with, and dying from, cancer desperately need that same attention—and funding.”
This mother learned this important truth in the hardest way possible: as a mother of a child with Diffuse Intrinsic Pontine Glioma, one of the deadliest of brain tumors, suffering from breast cancer herself. Several months after finishing her last breast cancer treatment in July 2008, she expressed her outrage in the lack of interest in childhood cancer:
“September 13, 2008 was our nation’s first Childhood Cancer Awareness Day. I didn’t see anything about it in the news, but I did hear about national “Talk Like a Pirate Day” a couple of days later. I made some calls to our local news stations, but to no avail…one of the story editors simply said, “So—what’s your event?” And again, later—”Pitch me a story.” So I tried giving them the important facts. 2,300 children die from cancer each year. One-quarter of children diagnosed with cancer will not survive. Federal support of childhood cancer clinical trial research is 30% less today than it was in 2003. But the facts generated no interest in national Childhood Cancer Awareness Day. I was told, “We put local news first.”
Okay. I can handle that. I have a list of local events. Like the shock of a family receiving a breast cancer diagnosis on an October Monday afternoon, and taking their six-year-old to the Emergency Room on Thursday only to be told, “There is a large area of swelling in the brainstem; we suspect a mass.” Or like a mother leaving the Pediatric Intensive Care Unit late one night to go home because she knows she needs to get a good night’s sleep before attending an Interdisciplinary Clinic early the next morning—where her own treatment plan will be recommended. Might there be any interest in a story about a local pastor, husband, and father being given the specifics of his son’s grim diagnosis and prognosis in one hospital while waiting for news of the specifics of his wife’s diagnosis and prognosis from the Cancer Center at another hospital?
Looking for a human interest story? How about a mother waking up in her child’s hospital room one morning, showering, and walking downstairs for her lumpectomy—while her husband takes over the duties of hospital parent and waits anxiously in his son’s room for news of his wife’s surgery? How about the same mother moving back into the hospital early on a Sunday morning four days later so that her husband, a pastor, can be in church, only to watch in disbelief as her fun-loving, active six-year-old, determined not to have an accident, becomes too weak to sit up to go to the bathroom on a bedside commode. What about the willingness of that little boy to allow the nurses to help him even with the most private of things—because he knows his mother is recovering from surgery and he is concerned for her well-being?
Not sensational enough? Let’s fast-forward to Saturday, November 24th, 2007, two days after Thanksgiving. A mother sits in a hospital room with her sleeping son. She ends a phone call because she hears an alarm she has never heard before, an alarm letting the nurses know that her son’s oxygen level is dropping. Soon the room is full, and it is determined that the child is disoriented, and then completely unresponsive. Somehow everyone moves with the child on that bed through the hallways to the Pediatric Intensive Care Unit where the intensivist begins the work of saving a precious life. The doctors ask, “Given his prognosis, do you want us to resuscitate him, if necessary?” The father, who has just arrived, breaks down in the unbelievable stress of the moment. The mother realizes the urgency of the situation, pushes emotions aside, and asks, “Do we know what is happening?” The answer is no. “Then, yes, we want you to do everything you can for him.” She stands at the foot of the bed with one of her son’s oncologists. Together, they watch the PICU teamwork, with purpose, like a machine. The mother steps outside the room only when the child is intubated. The drama continues, as the entire department revolves around that one room, that one little boy. The eyes of those outside the room—every nurse, every resident, every doctor—are looking in the same direction. The parents sign permissions as they are handed to them, and the work goes on. Everything seems to be happening in slow motion. Finally, the intensivist approaches. The child is critical, but stable, on life support.
This is the story of the first month of our lives in the pediatric cancer world. What will it take for people outside of the childhood cancer community to notice what is happening to our children? What will it take for everyone to understand the urgency of the situation? What will it take for the federal, state and local governments to finally engage in the fight? Will it be the cancer diagnosis of a celebrity’s child or the child of a political leader? Will it be the death of a child belonging to someone in the media? Will it be your child?”
In October 2013, this mother marked six years as a cancer survivor. In her words, “I am no longer the mother of a child with cancer; I am the mother of a child who died of cancer on December 4, 2009 at the age of 8.” We can only imagine her outrage, her sadness at the knowledge that modern medicine could save her life, but not the life of her child.
For this child to have the same chances of survival as his mother, we need to invest in research tailored for his specific type of cancer. Just as a child with a fever cannot be given adult ibuprofen, a child with cancer cannot be treated like a little adult with a smaller form of adult cancer. Why must childhood cancers be treated differently? First, children simply don’t get the same kinds of cancer as adults. Children can get cancer in their blood, their brain, their bones, their kidneys, their lymphnodes, or their soft tissues (just to list a few), but they do not get the adult cancers that receive the most attention from researchers and the media: lung, breast, prostate, and colon cancer. Second, childhood cancers tend to be more aggressive and fast-growing than adult cancers. Moreover, because of the aggressive nature of childhood cancers, and the fact that the symptoms are easily confused with normal childhood maladies, childhood cancers are more likely to be diagnosed in later stages, when the disease is more difficult to treat. Finally, because children’s bodies are still in a state of growth and development, they are much more sensitive to the toxic and harsh treatments required to fight the disease. Children who manage to survive their initial diagnosis are commonly diagnosed with secondary cancers directly stemming from their original treatment. And in many cases, the treatments used to fight either the original or the secondary cancer lead to severe long-term disabilities. Children’s sensitive bodies require medications and cures that target their disease, not their entire body.
Why do we tolerate the fact that a woman with breast cancer has a 98% chance of long-term survival, while her son with DIPG has less than a 30% chance of survival? Why do we tolerate the fact that a woman with breast cancer has more than triple the research resources devoted to her than is devoted to her child? Why do we tolerate the fact that in 2008, the year of this mother’s story, funding for pediatric cancer was $26.4 million, while funding for breast cancer research was $584 million? These are facts that we should not be tolerating, because they are intolerable. All children have the right to survive cancer in all its forms. The medical miracles seen in adult cancers can be mirrored in childhood cancers, but only if the same attention and funding is devoted to them as is devoted to adult cancers. Join us as we StepUp to increase awareness of this inequality. Join us as we StepUp to tell the world that cancer’s smallest victims need a larger share of the pie. What can you do? Share a post of Facebook and Twitter. Write to your congressman and remind them, beg them, to support increased funding for research on childhood cancers. Help us ensure that all children have a 100% chance of surviving childhood cancer.
There are many ways for you to help:
- A little bird will shout from the rooftops that kids deserve to be a higher priority. Tweet your members of Congress usingSoundOff with a new message each day. Here is an example tweet:
- I just sent a #SoundOff to my Reps in Congress about #StepUp. Would you hit this link and do it too? http://www.soundoffatcongress.org/nY2f
- Posting to Twitter on your own? That’s great! Please use the #StepUp hashtag so we can track our success. Here are some example posts:
- Step Up: More Funding for #ChildhoodCancer Research #StepUp http://www.soundoffatcongress.org/nY2f
- Children with cancer deserve more federal research funding. Tell Congress to #StepUp: http://www.soundoffatcongress.org/nY2f
- Increase appropriations for NCI #StepUp – More Funding for Childhood Cancer Research http://www.soundoffatcongress.org/nY2f
- Help us virtually storm Congress: Ask your Reps to #StepUp & support more funding for childhood cancer research. Please share!
- Email your Representatives (by clicking either of these links: House and Congress) and ask them to increase appropriations for NCI and reauthorize the Carolyn Pryce Walker Act.
- Change your Facebook and Twitter profile photos to the “StepUp” image
- Directly ask three friends to share the message with their representatives
Thirty Percent
30% – The Amount of GOG Federal Funding Cuts Over the Past Ten Years
Day 6: 30% – amount of COG federal funding cuts over past 10 years (adjusted for inflation)
Providing a Voice for the Voiceless – By S. Stephen Smith, age 17—written in memory of his 8-year-old brother Andrew
“The American Cancer Society estimates that 15,780 children and adolescents will be diagnosed with cancer in 2014. Cancer is the leading cause of death by disease for American kids. However, less than four percent of NIH funding is designated to pediatric cancer research every year. In 2007 my younger brother Andrew was diagnosed with diffuse intrinsic pontine glioma (DIPG), a rare, inoperable and terminal brain tumor. He was one of the thousands of American kids who are diagnosed with cancer annually. In 2012 the National Cancer Institute funded $208,070,156 worth of research for all types of childhood cancer combined compared with $602,728,719 for breast cancer research alone.
This is a societal injustice that is not made public because children do not have a voice. They are not represented in the media, government, or corporate worlds. They cannot organize massive fundraising drives for themselves, and they are not able to gain the attention of adults who can do something about their plight. Pharmaceutical companies stay away because there is no profit in pediatric cancer research, the government fails to step up, and our children—our neighborhood kids, and our schoolmates—are stuck with the cancer treatments we have been using for the last fifty years.
Something has to change. We can be the difference. Standing up, speaking out, holding firm and not backing down. It cannot be more applicable than now. Spread the word, state the facts and see the change. Without an increase in funding for childhood cancer, we will still be using the same old treatments fifty years down the road. Surely the children of our communities deserve better. I know my brother did.”
Although necessary, the plethora of numbers and statistical percentages surrounding discussions about money, budgets, and funding cuts can sometimes seem impersonal and difficult for us to connect to, but the dire repercussions of the statistics Stephen cited become horrifyingly real if we take the time to get to know some of the children who did not survive their battle with childhood cancer.
Our hope is that after reading the following heart-wrenching excerpts, and getting to know more about some of the brave little individuals whose lives were lost during the war against childhood cancer, the consequences of the 30% federal funding cuts for COG hospitals (over the past ten years) will no longer be discussed in abstract percentages, but rather in terms of the tangible loss of innocent lives.
Name: Aimee Lynn Dickey, DOB: 07/22/96, Diagnosed with DIPG: 09/27/07, Date of passing: 12/12/08
“Aimee started complaining of headaches in January, which became more severe over the next few months. During our initial trip to the doctor, prior to any tests being done, it was determined that she had migraines and she was given medication for her headaches. Aimee was a cheerleader and had several competitions between May and August—it was around this time that she began losing her balance, and started getting hic-ups even with just a sip of water. She then began to struggle with her breathing. After several more trips to the doctor’s office—again with no tests done, she was given acid reflux medicine, as well as asthma medicine. We were told that she was dehydrated and were given several antibiotics for an inner ear infection, which they claimed was responsible for the dizziness and loss of balance. Finally, at the end of August she began to vomit and needed much more sleep than in the past. She told me that the doctors were crazy, because the only thing wrong with her was that she had a brain tumor. I of course told her she was crazy, because “kids don’t get brain tumors.” Then she made a bet with me for $10.00 because she said she felt it growing.
September 25th, I took Aimee to see a new doctor; he did several neurological exams and referred us to a neurologist. The earliest appointment we could get was in October. Upon leaving the office Aimee began to vomit profusely, refused to go back in to see the doctor and just wanted to go home and sleep. She stayed home from school the next day, and slept and vomited off and on all day. Then on Thursday the 27th, Aimee woke up with an extreme headache but still wanted to go to school because it was picture day.
We began to ride our bikes and Aimee was swerving all over the road. I joked that she was going to get a DUI for her riding. She said instead that she was going to pass out—and she did. We rushed to the hospital and Aimee was immediately taken in for a CAT scan. A doctor came in and told me they saw a shadow on her brain and were taking her for an MRI. I was then taken to another room, where the doctor told me that Aimee had an inoperable brainstem tumor. At that point I sat in the room numb, and in total disbelief. How can my child have a brain tumor? This cannot be happening! I walked back into Aimee’s room, attempting to mask my inner panic, and saw that Aimee had her hand out, waiting for her $10.00.
Aimee was admitted for further testing and was immediately put on dexamethasone (a potent synthetic steroid) to reduce the swelling within her brain. Aimee’s neurosurgeon explained that Aimee had a DIPG, which was why surgery was not an option. He also told us that Aimee should not have lived long enough to be diagnosed and that her tumor was the worst they have ever seen, concluding with the grim statement that Aimee would likely only survive 6 months with radiation, if that long. Again, I was in shock.
Aimee spent a total of 54 days in the hospital. She responded very well to the radiation and was back to her old self before we were discharged. She was also weaned of the dexamethasone before we left the hospital. The only medication she was sent home with was oxycodone for pain. In April we learned that her tumor had progressed, and that she would have maybe 8-12 weeks left to live. At that appointment we were told that she could start a new trial. Aimee and I discussed it, and she asked, “What will this treatment do for me?” Answer: “Maybe extend your life by a few weeks, during which time you may be very ill.” She looked at me, then back at the doctor and said, “If I only have a short time left I would rather die holding my mother, rather than holding the toilet—keep your drugs.” A few weeks later Aimee woke with a severe headache, and was partially paralyzed on her right side, but Aimee was insistent about returning to school in September. She was entering the 7th grade in a brand new school in a new state and didn’t know anyone in her class. A few days after school started I found a letter that she had written to her classmates:
HI I AM AIMEE, I AM 12 YEARS OLD, AND I AM JUST LIKE YOU. I LOVE READING, MUSIC, GO-KART RACING, CHEERLEADING AND MAKING CRAFTS. YES I MAY BE SITTING IN A WHEELCHAIR, AND MY FACE MAY LOOK FUNNY AND TALK FUNNY, BUT PLEASE DON’T BE AFRAID OF ME BECAUSE YOU CAN NOT CATCH WHAT I HAVE. I HAVE A BRAIN TUMOR AND THE DOCTORS SAY I AM GOING TO DIE. BUT I JUST WANT TO BE AS NORMAL AS POSSIBLE JUST LIKE YOU. SO PLEASE DON’T BE AFRAID OF ME. I AM NOT AFRAID OF YOU EVEN WHEN YOU MAKE FUN OF ME. I WILL STILL BE YOUR FRIEND SO CAN YOU PLEASE BE MINE.”
Name: Caleb Wayne Spady, DOB: 1-7-98, Diagnosed DIPG: 4-3-08, Date of passing: 7-21-09
“Our son was 10 years old when he was diagnosed with DIPG. Like most 10 year old boys, he was active and vibrant—full of life. He lived life to the fullest and was happiest when he was playing baseball.
There weren’t many clinical trials available for children newly diagnosed with DIPG when Caleb was diagnosed on April 3, 2008. The only trial available via the pediatric oncology clinic easily accessible for us was a Phase II COG trial involving motexafin gadolinium as a radiosensitizer. We were told that radiation therapy was the only treatment that had even a remote a chance of working for kids with DIPG, which is why the focus of most clinical trials was to increase the effectiveness of radiation. This made sense to us, so we entered Caleb in the trial.
Each morning, Caleb received an infusion of the bright green motexafin gadolinium compound in the pediatric oncology clinic. Within a week of beginning the trial, Caleb began to develop unusual side effects. He became very sensitive to the sun; he felt a prickly sensation that quickly developed into full-fledged pain when he was outdoors. Within days of this, blisters began appearing on his face, hands, neck, arms and ears. At first they were just little water blisters. Soon, they became huge bubbles—some of them as large as a small apple on the backs of his hands. His fingernails turned a milky white and began to separate from his nail beds.
Throughout this time, despite a tremendous amount of discomfort, Caleb continued to play baseball. We saturated him in sun screen and covered his skin with cloth and bandages. The pain was intense. He had already been relegated from the position of shortstop (where he had played his entire life) to outfield, because his reaction time was slowing. Now he could hardly stand to be in the field. After the third out was called, he raced into the dugout where we had ice chests filled with cold and warm rags to wrap him in—one of the few efforts that brought him any relief. We rubbed topical anesthetic on his skin and, when it was time for him to hit, he wore an eye-patch on his left eye, and thick football lineman’s gloves to dull the pain of the blisters as his hands tightly gripped the bat.
The green chemicals gave his skin a green tint and even produced green stripes down his neck and back, and across his shoulders. Add the blisters, various bandages and big gloves and he looked like quite a character—hardly the accomplished and talented baseball player he was. There were times when ignorant fans or unknowing umpires made thoughtless comments. Still, he played. He was devoted to the game. Caleb was miserable while he was on the trial and for several weeks after it had concluded. We worked to heal the damage that had been done, but his skin was marred and scarred by the blisters and open wounds, and he never looked the same.
I greatly regret that we allowed him to suffer so—even required it of him. He never complained about the therapy; never once did he consider withdrawing from the trial. We believed it held promise and was the only hope we had of beating the evil disease. He was ready to fight from the moment he was diagnosed; he was a tough boy.”
Name: Hope Alizah Kimlee Fuller, DOB: 6/26/97, Diagnosed with DIPG: 7/29/09, Date of passing: 3/10/10
“In the first few days after diagnosis, things tend to be a blur. As you are still trying to process the words “average survival is less than 1 year” you begin to notice disturbing changes in your child–eye issues, balance issues, head ache, nausea, just to name a few. Treatment…well really at this point there is none. You are told that steroids and radiation will most likely shrink the tumor initially and help with symptom management, but this little “honeymoon period” is short-lived, and soon enough the tumor will begin to grow again. Various highly technical treatment options are discussed, but there is little (if any) data indicating that any of these painful and invasive treatments will actually extend your child’s life expectancy of the child beyond 24 months—and as a parent, you must take into consideration what your child’s quality of life would be during that time…
Initially you see the steroids as your saving grace. You hear the side effects of extreme hunger and weight gain as possibilities but with naïve confidence you think that you can control your child’s portions and just encourage healthier choices. There is no reason for significant weight gain for your child. Sleeplessness won’t be a problem because your child sleeps like a rock. Incontinence isn’t even mentioned in those early days. Muscle deterioration? No problem, your child is active and strong. Anger management has never been an issue at your house, tantrums are not acceptable.
My Hope was one of the children who (with the exception of 48 hours) were never off of the steroids. She gained over sixty pounds in just six months and lost the use of her right arm. She was able to walk assisted short distances until about five weeks before she died, but other than that, she was confined to a wheel chair. Her stretch marks were worse than any pregnant woman I’ve ever met and eventually those marks became open wounds in some areas. Hope never had the reprieve of a ‘honeymoon period.’ Hope saw no relief from the radiation. We watched in a state of helpless devastation as her tumor, which had barely shrunk at all, began to grow almost immediately, creating areas of necrosis that caused further harm to our beautiful girl. Through every nightmarish moment Hope was courageous. She continued to speak in terms of “when I get better” and “after treatment.” She attended therapy even when it hurt because she knew it was ‘good for her’. Hope was a hero.
We live in a world of constantly emerging technologies, and I believe that there are new, more effective cancer therapies on the horizon. I pray that your child will be the first of many long-term cancer survivors.”
These children represent just a few of the casualties in the war against childhood cancer. Their lives have become the collateral damage of merciless funding cuts, which have further restricted the alreadylimited number of clinical trial options available for children with cancer.
These children need better options—they should not have to choose between death and ineffective clinical trials that will reduce their quality of life to an unbearable level. Please join the #StepUp campaign as we lobby congress to secure increased funding for childhood cancer research through the National Cancer Institute (NCI).
You can support the #StepUp campaign by:
- Sharing a post on Facebook or Twitter, and asking friends to do the same
- Sending a letter to your Congressional Representative or Senator
- Tweeting directly at your Senator/Congressional Reps at the #SoundOff campaign website (#StepUp).
The war against childhood cancer will be lost without adequate funding for clinical research, but together we can tilt the scales toward victory, ensuring that no child’s life is cut short because of childhood cancer.
There are many ways for you to help:
- A little bird will shout from the rooftops that kids deserve to be a higher priority. Tweet your members of Congress usingSoundOff with a new message each day. Here is an example tweet:
- I just sent a #SoundOff to my Reps in Congress about #StepUp. Would you hit this link and do it too? http://www.soundoffatcongress.org/nY2f
- Posting to Twitter on your own? That’s great! Please use the #StepUp hashtag so we can track our success. Here are some example posts:
- Step Up: More Funding for #ChildhoodCancer Research #StepUp http://www.soundoffatcongress.org/nY2f
- Children with cancer deserve more federal research funding. Tell Congress to #StepUp: http://www.soundoffatcongress.org/nY2f
- Increase appropriations for NCI #StepUp – More Funding for Childhood Cancer Research http://www.soundoffatcongress.org/nY2f
- Help us virtually storm Congress: Ask your Reps to #StepUp & support more funding for childhood cancer research. Please share!
- Email your Representatives (by clicking either of these links: House and Congress) and ask them to increase appropriations for NCI and reauthorize the Carolyn Pryce Walker Act.
- Change your Facebook and Twitter profile photos to the “StepUp” image
- Directly ask three friends to share the message with their representatives
Ninety Percent
90% – The Number of Kids with Cancer Treated at COG (Children’s Oncology Group) Hospitals
Day 5: 90% – number of kids with cancer treated at Children’s Oncology Group (COG) hospitals
Children and adolescents with cancer are in a constant battle for their lives—and the front lines of this war are fought within the hospital walls where their treatments take place. The Children’s Oncology Group (COG) is the largest organization in the world devoted exclusively to childhood and adolescent cancer research, and includes a network of more than 200 children’s hospitals, universities, and cancer centers across North America, New Zealand, Australia, and Europe.
This group of hospital institutions collaboratively conducts much needed research and large-scale clinical trials with the goal of improving current treatment protocols and implementing innovative therapies for children with cancer.This year alone, more than 90% of the 15,760 children and adolescents diagnosed with cancer in the United States are cared for at Children’s Oncology Group member institutions, with estimates as to the number of children currently receiving cancer treatment at COG hospitals ranging from 30,000-40,000.
John Oliver (“Ollie”) Tetloff is one of the many children currently undergoing cancer treatment at a COG hospital, and the story of this courageous little boy’s battle with cancer is vividly depicted in a blog written by his mother, who often composes her blog posts during the many hours spent sitting by her son’s hospital bedside…

“Most kids in Alabama spend 180 days in school each year. Due to John Oliver’s cancer diagnosis, the accompanying intensive treatment plan, and his weakened immune system, he has missed his entire first-grade school year. Instead, my sweet boy has spent 180 nights in the hospital, and countless days visiting the outpatient oncology clinic for complete blood counts (CBCs), doctor exams, blood and platelet transfusions…and then there were the frantic trips to the Emergency Room to manage the frighteningly sudden onsets of fevers, pain, and nausea. That adds up to more than an entire school year of my son’s life spent within the confines of hospital walls. Rather than reading, playing at recess, and socializing with other children his age, Ollie’s daily schedule involved needle pokes, vomiting, more medicines than I ever thought possible, and a constant barrage of painful scans and tests.
Ollie was diagnosed with Stage-Four neuroblastoma (NB) at age six. He is seven years old now, and, as this particular type of cancer has an extremely high fatality rate, he is unlikely to celebrate his eighth birthday three months from now. Throughout this entire nightmarish experience, my greatest fear was to watch him suffer from the aggressive treatment plan all Stage-Four NB kids are subjected to, only to lose him. Heart-achingly, this seems to be our fate. To date, my brave little boy has withstood nine rounds of intensive chemotherapy, surgery, a bone marrow transplant, four weeks of daily radiation, immunotherapy, and MIBG therapy, which is a specialized molecular form of radiation that requires a weeklong stay in a lead-lined room (isolated from others due to radiation contamination). Yet despite all of these invasive treatments that have literally eaten away at his frail body, his cancer continues to grow. The cancer has now spread throughout his body—assaulting his spine and pelvis, taking away his ability to walk; infesting his lungs, causing respiratory distress; and invading his skull, threatening his eyes and brain. Over just the past three days, he has completely lost vision in his right eye. Despite our best tools and treatments, the cancer is winning.
 Obviously, these are difficult days, even when things go “well”—as parents of a child living with cancer, there is no reprieve from the fear and pain of watching your child suffer. But at this phase, we are too immersed in the daily task of living with cancer to dwell too much on the potential dangers lurking in the future. And not every day is terrible. Life goes on despite my fears. We get up each day, and do what we need to do in order to balance fighting the cancer and providing Ollie with the highest quality life possible. He is so much more than a cancer patient—he is a seven-year-old boy, and his childhood still needs nurturing and room to thrive. The only way for a child to spend an entire school-year in a hospital and not lose that precious sense of “being a kid,” is with the help of a compassionate medical team, dedicated to caring for Ollie in a manner that respects and preserves the integrity of his childhood.
Obviously, these are difficult days, even when things go “well”—as parents of a child living with cancer, there is no reprieve from the fear and pain of watching your child suffer. But at this phase, we are too immersed in the daily task of living with cancer to dwell too much on the potential dangers lurking in the future. And not every day is terrible. Life goes on despite my fears. We get up each day, and do what we need to do in order to balance fighting the cancer and providing Ollie with the highest quality life possible. He is so much more than a cancer patient—he is a seven-year-old boy, and his childhood still needs nurturing and room to thrive. The only way for a child to spend an entire school-year in a hospital and not lose that precious sense of “being a kid,” is with the help of a compassionate medical team, dedicated to caring for Ollie in a manner that respects and preserves the integrity of his childhood.
You may not think it at first, but the most insidiously spirit-dampening parts about the cancer treatment experience are the daily minutiae of everyday hospital life. One of Ollie’s most dreaded tasks is changing the dressing that covers his central line. An infection of the line or his blood is life-threatening for a child with a compromised immune system, so it must be done with the care and expertise of a nurse. And it hurts each and every week. The large bandage must be pulled off of Ollie’s sensitive, fragile skin, often covered with sores from the bandages, and then the entire area must be swabbed three times with alcohol, which is great to kill germs, but painful on raw skin and sores.
 Ollie worries about it all week, and dissolves into tears when the time finally comes. Even after fifty-two dressing changes, the look of pure fear in his eyes is always the same. Ollie’s only comfort in this experience is when he is allowed to remove the bandage himself. Doing so allows him to feel more in control of the process, and he can pull it off in a manner that minimizes the pain. This can be a rather painstaking endeavor, and to accomplish it we need a nurse who is willing to sit patiently by Ollie’s side, encouraging him to remove the bandage at his own pace, ensuring that the quality of care is not compromised. It is this consistently high level of patient care (even when it comes to the smallest of details) that helps us get through our days, and without which, our already fragile sense of hopeful persistence could easily disintegrate. When John Oliver is in pain, and we push the call button to request medicine, every second we spend waiting feels like an eternity. We need medical professionals who understand this, and who share our sense of urgency to help Ollie feel better. We have found this type of responsive, compassionate care from the doctor and nurses at our hospitals.
Ollie worries about it all week, and dissolves into tears when the time finally comes. Even after fifty-two dressing changes, the look of pure fear in his eyes is always the same. Ollie’s only comfort in this experience is when he is allowed to remove the bandage himself. Doing so allows him to feel more in control of the process, and he can pull it off in a manner that minimizes the pain. This can be a rather painstaking endeavor, and to accomplish it we need a nurse who is willing to sit patiently by Ollie’s side, encouraging him to remove the bandage at his own pace, ensuring that the quality of care is not compromised. It is this consistently high level of patient care (even when it comes to the smallest of details) that helps us get through our days, and without which, our already fragile sense of hopeful persistence could easily disintegrate. When John Oliver is in pain, and we push the call button to request medicine, every second we spend waiting feels like an eternity. We need medical professionals who understand this, and who share our sense of urgency to help Ollie feel better. We have found this type of responsive, compassionate care from the doctor and nurses at our hospitals.
When we were told of Ollie’s diagnosis, I had to google “neuroblastoma” just to learn about his specific cancer, so I obviously had no idea where he would receive the best treatment. But as I learned about the Children’s Oncology Group (COG) network structure, and that the COG protocols were based on decades of research, collaboration, and information-sharing across hospitals, my decision was made. Ollie has been treated at two COG hospitals, and each one has attended to the details of daily life with thought and care, making our time there as comfortable as possible. Sleep deprivation is a common problem when caring for a sick child, and yet I have had some of my best nights in the hospital, thanks to thoughtful and experienced nurses who have made the extra effort to attend to nighttime needs with minimal light and noise, anticipating the IV machine beeps and timing of medicines to keep nausea and pain at bay.
 Unfortunately, in the war against childhood cancer, cancer wins most of the battles; however, one of my favorite hospital memories occurred shortly after Ollie’s bone marrow transplant. He was isolated to a hall with eight hospital rooms, restrained by many rules to restrict contact with germs and other hazards while his immune system was wiped out and rebuilt. He was sad, bored, and suffering from mouth sores, seeming to lack interest in anything. The physical therapist came by, noticed his dejected temperament, and arranged a sticker scavenger hunt in the hallway. Ollie had to wear a mask and gloves to leave his room, and the stickers had to be wrapped in plastic to avoid any potential contamination, but it got him out of his room, walking through the little hallway, laughing and playing, even with an IV pole in tow. The sparkle renewed in his eyes was clear evidence that childhood took the victory on this one!
Unfortunately, in the war against childhood cancer, cancer wins most of the battles; however, one of my favorite hospital memories occurred shortly after Ollie’s bone marrow transplant. He was isolated to a hall with eight hospital rooms, restrained by many rules to restrict contact with germs and other hazards while his immune system was wiped out and rebuilt. He was sad, bored, and suffering from mouth sores, seeming to lack interest in anything. The physical therapist came by, noticed his dejected temperament, and arranged a sticker scavenger hunt in the hallway. Ollie had to wear a mask and gloves to leave his room, and the stickers had to be wrapped in plastic to avoid any potential contamination, but it got him out of his room, walking through the little hallway, laughing and playing, even with an IV pole in tow. The sparkle renewed in his eyes was clear evidence that childhood took the victory on this one!
When we learned that Ollie’s cancer was not responding to the frontline protocol, our world was once again thrown into chaos, but due to the collaborate nature of the COG, our oncologist was able to consult with colleagues around the country in a timely manner, and we were able to find an alternative treatment only a few hours away. Since that time, the two institutions have remained in close contact, allowing us to receive treatments at home when it is available, and quickly transitioning back into our secondary hospital when it was necessary.
 My son’s failing health is not due to incompetent care or denied access—it is directly linked to insufficient funding for childhood cancer research. It is almost impossible for me to fathom that these already inadequate funds are at risk of further cuts. The horrendous suffering of my sweet seven-year-old boy is due to harsh and ineffective treatments; any chance he has of survival is because of the high quality of care we have received at Children’s of Alabama and Children’s Healthcare of Atlanta. I’d invite any congressperson to spend the night on either of these oncology floors and witness firsthand the diligent and committed work of the medical teams, and the profound and heartbreaking suffering of their tiny patients. It is very clear that no funding can be spared, and that to save our children from pain and death, we must prioritize funding for children’s hospitals and cancer research centers. No one should have to watch their child die a slow and painful death when there is the possibility of a cure.“
My son’s failing health is not due to incompetent care or denied access—it is directly linked to insufficient funding for childhood cancer research. It is almost impossible for me to fathom that these already inadequate funds are at risk of further cuts. The horrendous suffering of my sweet seven-year-old boy is due to harsh and ineffective treatments; any chance he has of survival is because of the high quality of care we have received at Children’s of Alabama and Children’s Healthcare of Atlanta. I’d invite any congressperson to spend the night on either of these oncology floors and witness firsthand the diligent and committed work of the medical teams, and the profound and heartbreaking suffering of their tiny patients. It is very clear that no funding can be spared, and that to save our children from pain and death, we must prioritize funding for children’s hospitals and cancer research centers. No one should have to watch their child die a slow and painful death when there is the possibility of a cure.“
Clinical research has demonstrated that children and adolescents treated at specialized children’s cancer centers (as opposed to local hospitals), have better treatment outcomes. A children’s cancer center is staffed with oncology healthcare teams that specialize in the diagnosis and treatment of childhood and adolescent cancers, which is highly important because children are not just “little adults” who can successfully be treated with lowered doses of adult cancer treatments.
The COG’s unparalleled collaborative research efforts and nearly 100 active clinical trials provide the information and support needed to answer crucially important, life-saving clinical questions in the fight against childhood cancer. These trials are specifically designed to reflect the unique treatment needs and responses of a child’s body, and include investigations into the underlying biology of different types of childhood cancers and the discovery of new and emerging treatments.
The COG is funded by the National Cancer Institute (NCI), and upholds the rigorous quality assurance standards the NCI has set forth. Federal funding for COG hospitals has been cut by 30% over the past decade, which has decreased the number of potentially lifesaving clinical trials for children like John Oliver. We are asking you to become allies of the children bravely fighting against a cunning and merciless enemy that is wreaking havoc on their innocent little bodies, causing unspeakable pain and suffering. Please join us as we lobby congress to secure increased funding for childhood cancer research through the National Cancer Institute (NCI).
You can support the #StepUp campaign by:
- Sharing a post on Facebook or Twitter, and asking friends to do the same
- Sending a letter to your Congressional Representative or Senator
- Tweeting directly at your Senator/Congressional Reps at the #SoundOff campaign website (#StepUp).
The war against childhood cancer will be lost without adequate funding for clinical research, but together we can tilt the scales toward victory, ensuring that no child’s life is cut short because of childhood cancer.
There are many ways for you to help:
- A little bird will shout from the rooftops that kids deserve to be a higher priority. Tweet your members of Congress using SoundOff with a new message each day. Here is an example tweet:
- Posting to Twitter on your own? That’s great! Please use the #StepUp hashtag so we can track our success. Here are some example posts:
- Step Up: More Funding for #ChildhoodCancer Research #StepUp
- Children with cancer deserve more federal research funding. Tell Congress to #StepUp:
- Increase appropriations for NCI #StepUp – More Funding for Childhood Cancer Research
- Help us virtually storm Congress: Ask your Reps to #StepUp & support more funding for childhood cancer research. Please share!
- Email your Representatives (by clicking either of these links: House and Congress) and ask them to increase appropriations for NCI and reauthorize the Carolyn Pryce Walker Act.
- Change your Facebook and Twitter profile photos to the “StepUp” image
- Directly ask three friends to share the message with their representatives